Falls Prevention
Falls remain one of the most common and serious risks facing frail older adults, particularly those living in care homes or receiving community-based support. Despite this, falls are often accepted as “inevitable” with ageing. The evidence tells us otherwise.
This blog draws directly from our falls prevention training and community physiotherapy experience to outline why falls happen, what actually reduces risk, and how physiotherapy plays a central role in prevention and recovery.
Why falls matter
Around one in three adults over the age of 65 will fall each year, with rates rising significantly in care home environments. Falls are not harmless events.
The impact is wide-ranging:
Physical consequences include fractures, head injury, pain, reduced mobility, and loss of independence.
Psychological effects such as fear of falling often lead to activity avoidance, deconditioning, and further falls.
Financial and system pressures increase through hospital admissions, long-term care needs, and increased staffing ratios.
Falls are also the second leading cause of accidental death worldwide in older adults. Prevention is therefore a safety issue, not a “nice to have”.
Understanding why older people fall
Falls rarely have a single cause. They usually result from a combination of intrinsic (person-related) and extrinsic (environmental or system-related) factors.
Intrinsic risk factors commonly include:
Muscle weakness and reduced power
Poor balance and altered gait
Visual impairment
Long-term conditions such as Parkinson’s disease, stroke, arthritis, or dementia
Cognitive impairment and reduced insight
Fear of falling
Orthostatic hypotension
Foot problems and inappropriate footwear
Urinary urgency or incontinence
Extrinsic risk factors often include:
Poor lighting
Trip hazards and clutter
Unsuitable furniture height or design
Incorrect or poorly maintained walking aids
Medication side effects
Sedentary routines, especially overnight
Inadequate supervision during higher-risk activities
Effective falls prevention depends on recognising how these factors interact for each individual.
Exercise: the strongest evidence we have
Exercise is one of the most effective interventions for reducing falls risk in older adults.
Well-designed strength and balance programmes can:
Increase muscle strength and bone density, even in very old or frail individuals
Improve balance reactions and postural control
Improve posture and walking pattern
Increase confidence and reduce fear of falling
Improve cognition and participation in daily activities
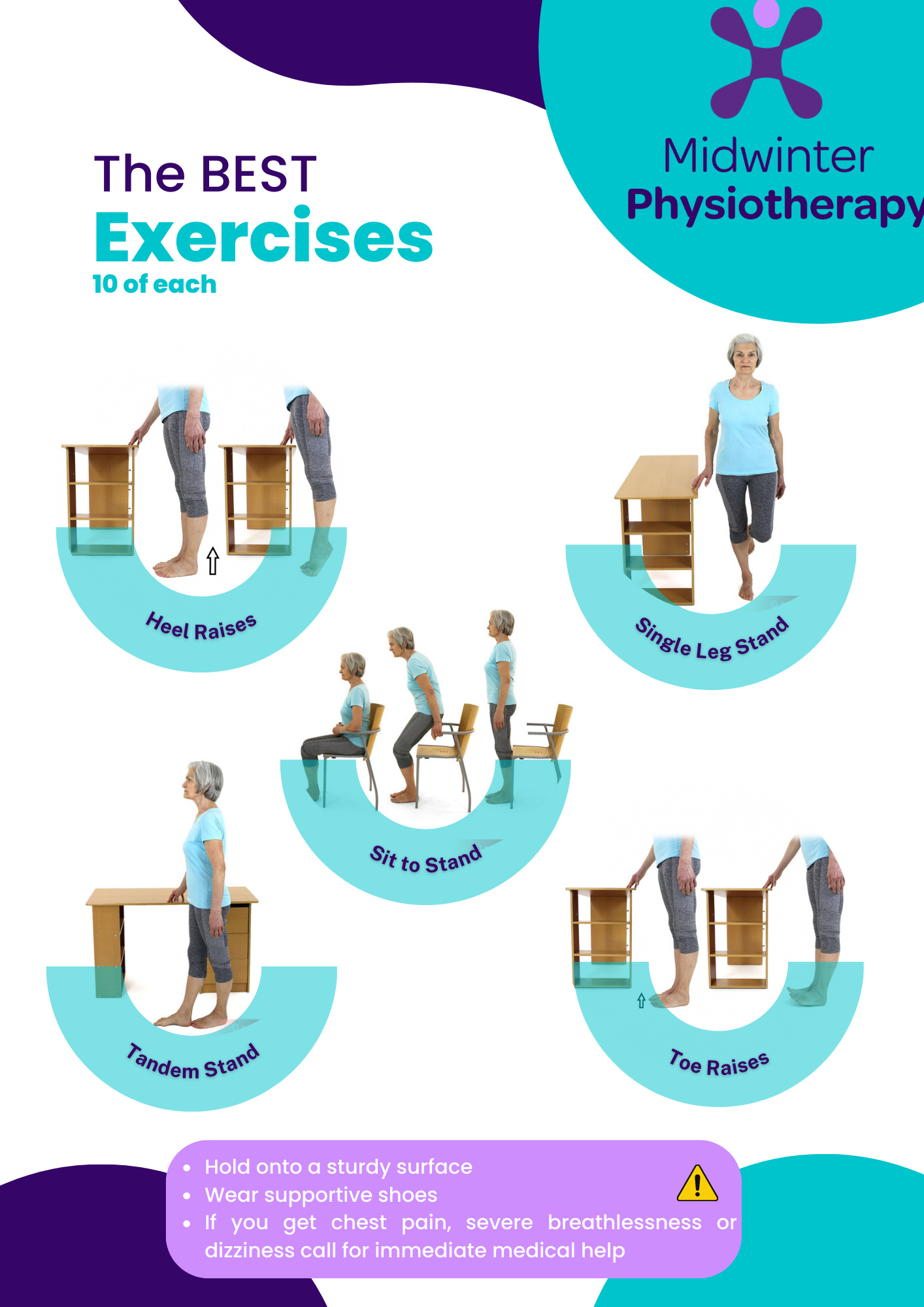
Physiotherapy-led programmes focus on functional movement, such as sit-to-stand, walking, reaching beyond the base of support, and safely challenging balance. These are not generic classes; they are tailored to ability, health conditions, and goals.
Exercise is prevention, not rehabilitation alone.
The environment matters more than people think
Environmental modification is one of the quickest ways to reduce risk, yet it is often overlooked or poorly implemented.
Simple but effective changes include:
Adequate lighting, especially at night
Grab rails and handrails where transfers occur
Non-slip, even flooring
Removal of trip hazards
Stable furniture at correct heights
Correct chair height to allow safe standing
Properly fitted walking aids
Accessible bedside tables and personal alarms
Avoiding trailing or baggy clothing
These changes reduce risk immediately and reduce physical strain on staff supporting mobility.
Medication and falls risk
Certain medications significantly increase falls risk through effects on blood pressure, alertness, coordination, and reaction time.
High-risk medication groups include:
Sedatives and hypnotics
Antidepressants and antipsychotics
Antihypertensives
Opioid analgesics
Antiepileptic drugs
Anticholinergic medications
Polypharmacy in general
Regular medication review, particularly after a fall or change in mobility, is essential. Physiotherapists often identify postural hypotension or mobility changes that should trigger review.
The role of staff education and culture
Falls prevention is not achieved through paperwork alone. Staff confidence, knowledge, and consistency are critical.
Effective training includes:
Understanding individual falls risk
Recognising early warning signs
Safe use of walking aids
Clear post-fall protocols
Confidence in rehabilitation and graded activity
Communication that reduces fear rather than reinforces dependency
A strong falls prevention culture reduces workload, reduces staff injuries, and supports residents to remain as independent as possible.
What to do if a fall occurs
Not all falls can be prevented, but the response matters.
Immediate priorities include:
Checking for injury
Avoiding rushed or unsafe lifting
Using agreed post-fall assessment protocols
Monitoring for delayed symptoms
Reporting and reviewing contributing factors
Where appropriate, individuals can be supported to get up safely using a structured approach, reducing panic and unnecessary injury.
Physiotherapy after a fall
Post-fall physiotherapy focuses on more than “getting someone walking again”.
Key elements include:
Detailed mobility and balance assessment
Identification of new or previously hidden risk factors
Targeted strengthening and balance work
Rebuilding confidence and reducing fear avoidance
Education for both the individual and their support network
Prevention planning to reduce future falls
Early intervention after a fall reduces long-term dependency and repeat incidents.
Why this matters for care teams
When falls prevention is done well:
Staff feel more confident and skilled
Physical strain and back injuries reduce
Residents require less hands-on support
Fear-driven behaviours reduce
Workload becomes more manageable
The need for 2:1 care often reduces
Falls prevention is not about restriction. It is about enabling safe movement.
Final thoughts
Falls are not an inevitable part of ageing. They are a clinical risk that can be reduced through evidence-based physiotherapy, environmental awareness, medication review, and skilled support.
In community and care home settings, physiotherapy plays a central role in keeping older adults mobile, confident, and safe; not just after a fall, but long before one happens.